

Mount Sinai Hospital: (305) 921-4679
Aventura Hospital: (305) 604-3216
Memorial Hospital: (305) 604-3216
Joints wear down over time causing stiffness and pain. Cartilage is the interface padding between two bones in the joint that allows smooth gliding and movement. Overtime, the cartilage can become worn-out and thin. Either systemic factors or the normal “wear-and-tear” of repeated use can trigger an inflammatory response that can alter and ultimately destroy the tissues (cartilage and bone) of the joint.
Patients with arthritis usually experience pain or weakness when doing daily tasks. These symptoms can be triggered by normal tasks such as opening jars and grabbing items.
Arthritis of the joints of the wrist and hands is very common, particularly in the thumb, and several treatment options exist including: medications, splinting, hand therapy, injections, and surgery. Surgery is usually recommended in severe cases or when there are issues with joint function. Sometimes joint replacement is recommended in cases where alternative, less invasive methods have failed.
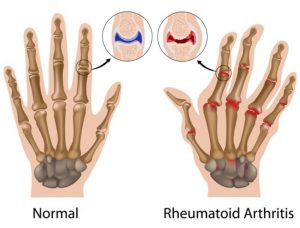
If you would like more information on arthritis, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
The Carpal Tunnel is a canal in the wrist bound by bones and ligaments through which a multitude of nerves pass on their way to the hand. Carpal tunnel syndrome is one of the more common disorders of the hand and wrist. It occurs from nerve compression of the nerves in this tunnel in the wrist. The median nerve is usually the nerve affected. The doctor can identify if you suffer from carpal tunnel syndrome by a combination of your symptoms cluster and a physical exam. Additionally, to confirm the diagnosis objectively, a nerve study—requiring a referral to a neurologist—is usually recommended.
When the median nerve is compressed, this may cause pain, numbness, tingling, weakness, cramps, or clumsiness in the hand. Most people experience these symptoms in the thumb, index, middle, and ring fingers. Overall, it has been noted that the pain gets worse at night.
Treatment options include medications, splinting, injection, or surgery. Surgery involves releasing the ligament thereby enlarging the carpal tunnel and thus, giving the nerve more space. Surgery can be performed “open” requiring a 2-3 cm incision on the wrist or “endoscopic” which is a minimally invasive technique with a smaller 1 cm incision allowing for quicker recovery and less down time. In most cases, this can be done with just mild sedation and local anesthesia.
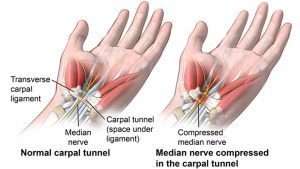
If you would like more information on carpal tunnel syndrome, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
Cubital tunnel syndrome, similar to carpal tunnel syndrome, but is caused by compression of a nerve in the elbow. This causes numbness and/or tingling typically in the ring and small fingers.
People with cubital tunnel typically experience pain on the inside of their elbow. Additionally, due to the compression on ulnar nerve, people notice a weaker grip, and difficulty moving certain fingers especially the ring and/or little finger.
Treatment may involve using an elbow pad, medications, occupational therapy, or surgery. This surgery is usually done in a minimally invasive technique, also known as endoscopic, utilizing a smaller than standard incision. A camera is then used to visualize the structures that compress the nerve, followed by releasing them. Overall, the endoscopic procedure allows quick recovery and minimal down time. In most cases, this can be done with just mild sedation and local anesthesia.
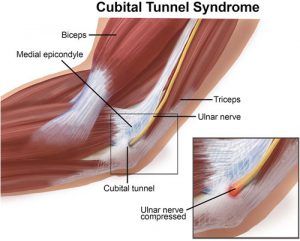
If you would like more information on cubital tunnel, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
Through repetitive movements of the thumb and wrist, the two tendons involved in these movements can swell and put pressure on nearby nerves causing pain known as De Quervain’s tenosynovitis. This pain is the result of inflammation and irritation from the friction of the thumb tendons against the bone.
Patients with De Quervain’s tenosynovitis typically have swelling at the base of the thumb, and numbness at the back of the thumb and index finger. Other symptoms usually include pain with thumb function.
De Quervain’s tenosynovitis can usually be treated without surgery. Through the use of anti-inflammatory medications, splinting, topical creams, hand therapy, and/or steroid injections. In rare cases, surgery may be necessary to release the tendon and relieve symptoms.
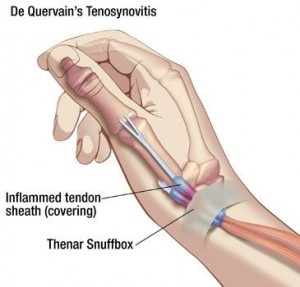
If you would like more information on De Quervain’s Tenosynovitis, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
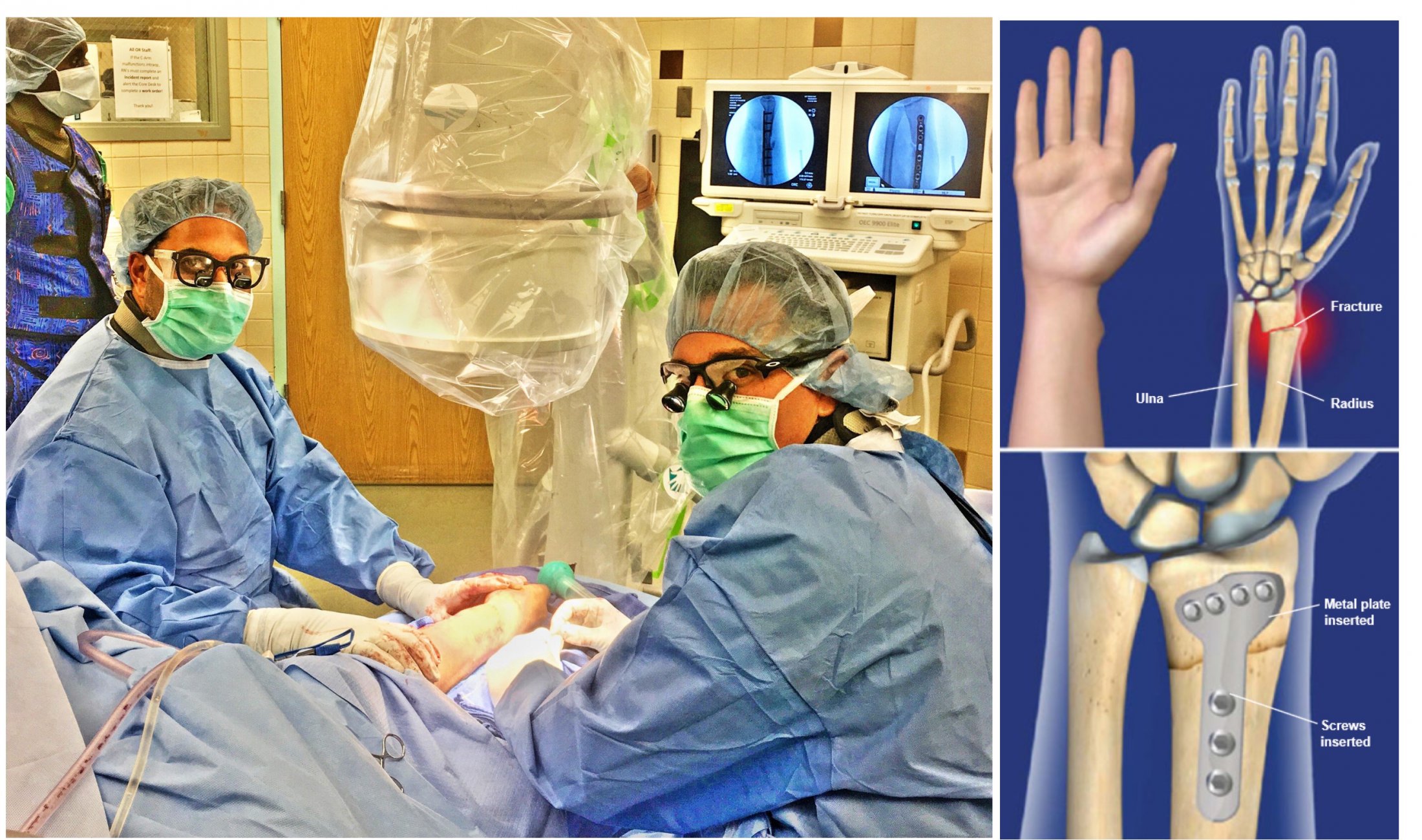
Your forearm has two bones, the radius and ulna. The larger of the two bones is called a radius, and this is often susceptible to trauma. In fact, from any fall or motor vehicle accident may cause a break of the wrist. This is sometimes called a distal radius fracture. Often times the term fracture and break are used interchangeably in the healthcare field as they mean the same thing.
A broken wrist usually results in immediate pain, bruising, and swelling.
Certain fractures may be treated non-operatively in a cast or a splint. Traditionally, wrist fractures were kept in an above elbow cast for 2 to 3 weeks, followed by another 4 weeks of casting below the elbow. In contrast, modern techniques allow for no casting after surgery. To address the fractured bone, your surgeon will use a plate and screws, resulting in an early range of motion and minimizing post-operative down time. Overall, operative treatment can eliminate the need for an uncomfortable cast in the South Florida heat. The key to a great outcome is appropriate hand therapy after surgery done by a certified hand therapist. After your surgery, your doctor and certified hand therapist will work as a team to ensure your return back to daily tasks as soon as possible.
If you would like more information on distal radius fracture, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
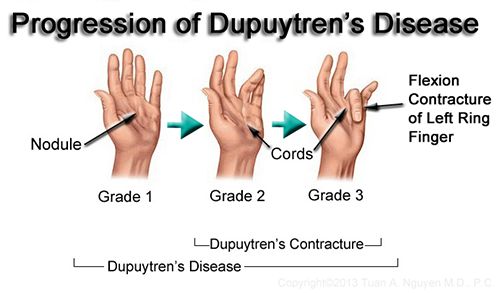
Your hand has fascia, a fibrous layer that connects skin to muscle. When the fascia thickens and tightens over time, the finger(s) may be pulled inward towards the palm resulting in a flexion contracture as the finger(s) lose mobility. Eventually the finger(s) cannot be completely straightened.
Patients with Dupuytren’s contracture develop symptoms over the course of several years. During the first grade, some people notice nodules, or small lumps at the palm of the hand, that are tender to touch. The second grade is noted when the nodules become thick and form cord-like tissue under the skin. In turn, the finger may be difficult to straighten or spread apart. The third degree is classified when one or more fingers are pulled inward toward the palm causing a contracture.
Sometimes this condition may not affect your hand function so treatment may not be necessary. If the hand function is affected, then injections or surgery can be used to address the contracture.
If you would like more information on dupuytren contracture, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
The forearm is between the wrist and the elbow, and it has two bones: the radius and ulna. A forearm fracture may result from any fall, participation in contact sports, or motor vehicle accident. Lastly, you may find that the term fracture and break are used interchangeably in the healthcare field as they mean the same thing.
A forearm fracture usually results in immediate pain, bruising, and swelling. You may also notice one arm shorter than the other.
Certain fractures may be treated non-operatively in a cast or a splint. Traditionally, fractures were kept in an above elbow cast for 4 weeks. In contrast, modern techniques now allows for no casting no casting after surgery. Most of these fractures require surgery with a plate(s) and screws, resulting in an early range of motion and minimizing post-operative down time. Overall, operative treatment can eliminate the need for an uncomfortable cast in the South Florida heat. The key to a great outcome is appropriate hand therapy after surgery done by a certified hand therapist. After your surgery, your doctor and certified hand therapist will work as a team to ensure your return back to daily tasks as soon as possible.
If you would like more information on forearm fracture, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
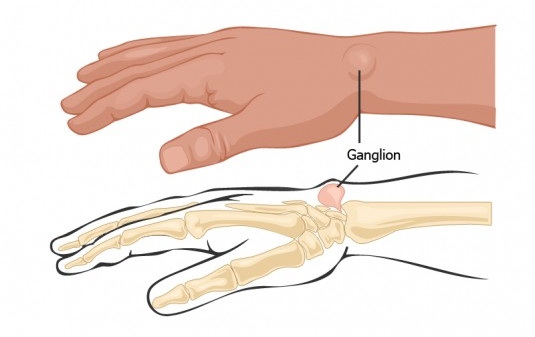
A ganglion cyst is a benign cystic mass, which oftentimes presents in the wrist or hand. The mass usually presents as small “pea-sized” but usually enlarges over time. The mass is cystic, in that it contains joint fluid, which is trapped outside the joint through a one way valve mechanism. The cystic mass contains joint fluid, which is trapped outside the joint space through a one-way valve effect which allows the fluid to come out of the joint space, but is prevented from flowing back.
Ganglion cysts most commonly develop along the tendons or joints of the wrist or hand. Patients may also notice the fluid vary in size. Based on the position of the cyst, pain may result if the mass presses against a nearby nerve. Additionally, some people may experience tingling, numbness, and stiffness.
The fluid can sometimes be removed with a needle, but oftentimes this treatment is only temporary as the cyst usually reoccurs. The best way to make sure the cyst does not reoccur is to have it surgically removed.
If you would like more information on ganglion cyst, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
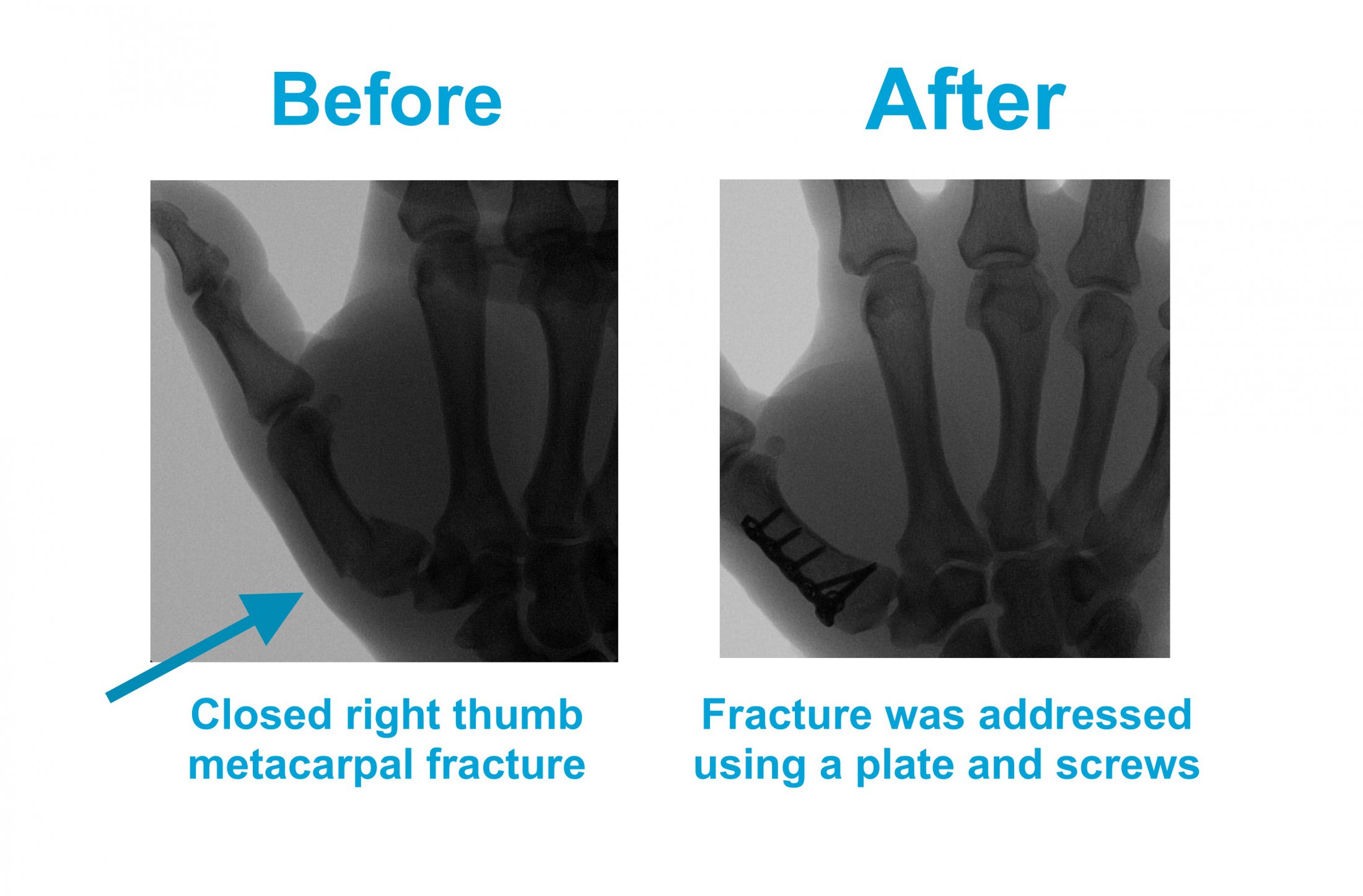
Hand and finger fractures are common in people who participate in sports or who are involved in any type of trauma to the upper extremity. Fractures to the bones in the hands (metacarpals) or to those of the fingers (phalanges) may cause the hand to become painful, swollen or anatomically distorted. The only way to know the difference between a “sprain” and a “fracture” is with an X-ray. Overall, you may find that the term fracture and broken-bone are used interchangeably in the healthcare field as they mean the same thing.
A fracture in the hand or finger usually results in immediate pain, bruising, swelling and may lead to distortion in the way the fingers or hand usually looks anatomically, if significant displacement of the bones is associated with the fracture.
Casting or splinting may be appropriate for treatment. Most of these fractures require surgery with the insertion of pins or small metal rods into the fractured bones, or the placement of plates and screws in order to hold the fractured bones in the correct anatomical position. Such surgery to address the fracture is usually done with mild sedation and local anesthesia, and does not require you to be put to sleep. The key to a great outcome and full range of motion of joints involved is appropriate postoperative hand therapy,done by a certified hand therapist.
If you would like more information on Finger Fractures, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
Hand and finger infections are relatively common. They can occur from animal/insect bites, or even minor trauma in those with medical conditions such as diabetes. This is caused from bacteria entering from the outside environment and causing infection in deeper tissues beneath the skin.
Hand or finger infections usually present with redness, stiffness, swelling and pain, particularly with joint function. Constitutional symptoms such as fever and chills usually indicate concerning progression of the infection.
It is critical to treat these infections early and in a timely manner to prevent permanent damage and contracture (stiffness) or progression of the infection up the extremity. Sometimes early infections are treated with antibiotics alone, but most times proper treatment requires a combination of antibiotics with surgical drainage.

If you would like more information on finger and hand infections, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
The reasons for shoulder pain are many including things such as systemic health conditions such as arthritis, trauma, overuse of the joint leading to tendon tears or disruption of the labrum (the “speed bump” of the shoulder which prevents the shoulder from dislocation).
Due to the various causes of shoulder pain, it is best to consult with your doctor for a comprehensive work-up in order to adequately determine the cause. To fully address the shoulder pain you are experiencing, a full medical work up including X-rays, MRI, is usually indicated. steroid injections, and/or physical therapy
The treatment for shoulder pain is determined by the diagnosis. Initially, your surgeon will always try to maximize non-operative treatments, and perform surgery as a last resort or when non-operative treatment is not effective. Some non-operative treatment modalities include steroid injections, physical therapy and strengthening exercises. When noninvasive modalities fail, your doctor will discuss surgery. Shoulder surgeries are almost always done non-invasively using arthroscopic techniques.

If you would like more information on shoulder pain, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
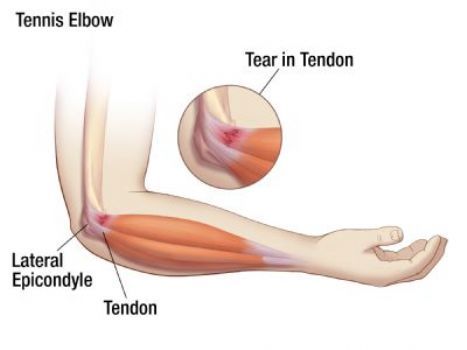
Tennis elbow is also known as lateral epicondylitis, and is usually the results of overuse of the elbow from repetitive movements of the wrist and arm from certain activities such as playing tennis. Interestingly, athletes are not the ones who are diagnosed with tennis elbow. Rather people whose job requires repetitive movements, such as plumbers, painters, or butchers are most commonly diagnosed with this condition.
Through the repetitive movements of the arm, small micro tears in the tendon thereby causing the pain. Most patients initially experience pain on the outside of the elbow that then radiates to the forearm and wrist.To identify if you have tennis elbow, your doctor will do a physical exam by applying pressure and ask you to move your elbow, wrist, and fingers in order to elicit and reproduce your symptoms.
The combination of rest and anti-inflammatory medication may help relieve the pain for mild cases. Additionally, your doctor may recommend physical therapy to help strengthen the muscles of the forearm. Otherwise, this can be treated in the office with a new state of the art technique, which involves the removal of the affected inflamed tendon fibers and which often leads to excellent results if the properly chosen patients.
If you would like more information on tennis elbow, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
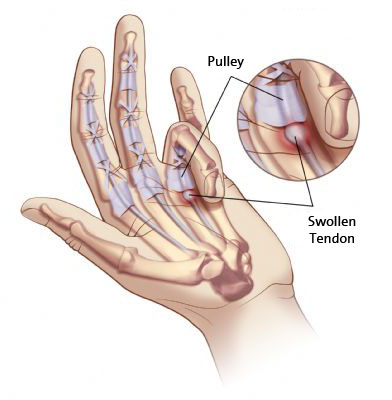
Trigger finger is a condition where thickening of the finger tendons cause the finger to “catch” or get stuck while the patient attempts to straighten the affected finger. Tendons are rope-like structures that connect muscles to bone and allow for joint function. With repetitive movements, the tendons in the finger(s) can become inflamed and cause “catching” type symptoms, but eventually can “lock” the finger(s) in place.
Repetitive movement of the tendon causes inflammation. You may notice your finger(s) getting stuck or locking into place as you try to move them.
To help relieve the symptoms, the doctor may recommend a steroid injection as well as anti-inflammatory medications. To allow the tendon to glide smoothly once again, surgical release of the tendon may be required. During the operation, your surgeon will widen the opening of the tendon allowing for better mobility of the finger. While this surgery is done in a hospital setting, you should be able to go home that day as this is an outpatient procedure.
If you would like more information on trigger finger, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
Arthroscopy allows the surgeon to view inside of your wrist joint without making a large open incision. Not only is this procedure diagnostic, but it also allows for certain corrective treatment interventions. Procedures that may be done through the scope includes removal of loose tissue, ligament repair, ganglion cyst removal, synovectomy, or TFCC (triangular fibrocartilage complex) repair. The recovery time for most arthroscopic procedures is quicker than open procedures, allowing patients to return to work and function sooner, rather than later.
If you would like more information on wrist arthroscopy, we invite you to review an educational website endorsed by the American Academy of Orthopaedic Surgeons.
© MOSA Surgery. All Rights Reserved. | Accessibility Policy
Last Updated: January 26th, 2021 11:03 AM